Hypo tropic cardiac mayopathi
Hypertrophic cardiomayopathi
Hypertrophic cardiomyopathy is a disease of the myocardium (the muscle of the heart)
in which a portion of the myocardium is hypertrophied (thickened) without any obvious cause. It
is perhaps most well known as a leading cause of sudden cardiac death in young athletes. The occurrence of
hypertrophic cardiomyopathy is a significant cause of sudden unexpected cardiac
death in any age group and as a cause of disabling cardiac symptoms. Younger
people are likely to have a more severe form of hypertrophic cardiomyopathy
HCM is frequently asymptomatic until sudden cardiac death, and for
this reason some suggest routinely screening certain populations for this disease.A cardiomyopathy is a primary disease that affects the
muscle of the heart. With hypertrophic cardiomyopathy (HCM), the sarcomeres (contractile elements) in the heart
replicate causing heart muscle cells to increase in size, which results in the
thickening of the heart muscle. In addition, the normal alignment of muscle
cells is disrupted, a phenomenon known as myocardial disarray. HCM also causes disruptions of the electrical
functions of the heart. HCM is most commonly due to a mutation in one of 9
sarcomeric genes that results in a mutated protein in the
sarcomere, the primary component of the myocyte (the muscle cell of the heart).
While most literature so far focuses on European, American, and
Japanese populations, HCM appears in all racial groups. The prevalence of HCM
is about 0.2% to 0.5% of the general population.
Myosin heavy chain mutations are associated with development of
familial hypertrophic cardiomyopathy.
Signs and symptoms
The clinical course of HCM is variable. Many patients are
asymptomatic or mildly symptomatic. The symptoms of HCM include dyspnea (shortness of breath), chest pain
(sometimes known as angina), uncomfortable awareness of the heart beat (palpitations), lightheadedness, fatigue, fainting (called syncope) and sudden cardiac death. Dyspnea is largely due to increased stiffness of the left ventricle,
which impairs filling of the ventricles and leads to elevated pressure in the
left ventricle and left atrium. Symptoms are not closely related to the
presence or severity of an outflow tract gradient. Often, symptoms mimic those
of congestive heart
failure (esp. activity
intolerance & dyspnea), but treatment is very different. To treat with
diuretics (a mainstay of CHF treatment) will exacerbate symptoms in
hypertrophic cardiomyopathy by decreasing ventricular volume and increasing
outflow resistance.
Risk factors for sudden death in individuals with HCM include a
young age at first diagnosis (age < 30 years), an episode of aborted sudden
death, a family history of HCM with sudden death of relatives, specific
mutations in the genes encoding for troponin T and myosin, sustainedsupraventricular or ventricular
tachycardia, ventricular septal
wall thickness over 3 cm, hypotensive response to exercise,
recurrent syncope(especially in children), and bradyarrhythmias
(slow rhythms of the heart).
Genetics Genetics
Genetics
Hypertrophic cardiomyopathy is inherited as an autosomal dominant trait and is attributed to mutations in
one of a number of genes that encode for one of the sarcomere proteins.
About 50-60% of patients with a high index of clinical suspicion
for HCM will have a mutation identified in at least 1 of 9 sarcomeric genes.
Approximately 45% of these mutations occur in the β myosin heavy chain gene on chromosome 14 q11.2-3, while approximately 35%
involve the cardiac myosin binding protein C gene. Since HCM is typically
an autosomal dominanttrait, children of an HCM parent have 50% chance
of inheriting the disease-causing mutation. Whenever a mutation is identified
through genetic testing, family-specific genetic testing can be used to
identify relatives at-risk for the disease (HCM Genetic Testing Overview). In individuals without a family history of
HCM, the most common cause of the disease is a de novo mutation of the gene that produces the β-myosin
heavy chain.
An insertion/deletion polymorphism in the gene encoding for angiotensin converting
enzyme(ACE) alters the
clinical phenotype of the disease. The D/D (deletion/deletion) genotype of ACE
is associated with more marked hypertrophy of the left ventricle and may be
associated with higher risk of adverse outcome
Pathophysiology
Individuals with HCM have some degree of left ventricular
hypertrophy. Usually this is an
asymmetric hypertrophy, involving the inter-ventricular septum, and is known as
asymmetric septal hypertrophy. This is in contrast to the concentric
hypertrophy seen in aortic stenosis or hypertension. About two-thirds of individuals with HCM have asymmetric septal
hypertrophy.
About 25% of individuals with HCM demonstrate an obstruction to
the outflow of blood from the left ventricle during rest. In other individuals
obstruction only occurs under certain conditions. This is known as dynamic outflow
obstruction, because the degree of obstruction is variable and is dependent on
the amount of blood in the ventricle immediately before ventricle systole (Contraction)
Dynamic outflow obstruction
|
Echocardiogram
demonstrating systolic anterior motion of the anterior leaflet of the mitral
valve
|
|
Dynamic outflow obstruction (when present in HCM) is usually due
to systolic anterior motion of the anterior leaflet of the mitral valve. Systolic anterior motion of the mitral valve
(SAM) was initially thought to be due to the septal subaortic bulge, narrowing
the outflow tract, causing high velocity flow and a Venturi effect—a local underpressure in the outflow tract. Low
pressure was thought to suck the mitral valve anteriorly into the septum. But
SAM onset is observed to be a low velocity phenomenon: SAM begins at velocities
no different from those measured in normals Hence, the magnitude and
importance of Venturi forces in the outflow tract are much less than previously
thought, and Venturi forces cannot be the main force that initiates SAM.
Recent echocardiographic evidence indicates that drag, the pushing
force of flow is the dominant hydrodynamic force on the mitral leaflets In
obstructive HCM the mitral leaflets are often large and are
anteriorly positioned in the LV cavity due to anteriorly positioned
papillary muscles that at surgery are often "agglutinated" onto
the LV anterior wall by abnormal attachments
The mid-septal bulge aggravates the malposition of the valve and
redirects outflow so that it comes from a lateral and posterior
direction. The abnormally directed outflow may be visualized behind and
lateral to the enlarged mitral valve, where it catches it, and pushes it into
the septum There is a crucial overlap between the inflow and outflow
portions of the left ventricle . As SAM progresses in early systole the
angle between outflow and the protruding mitral leaflet increases. A greater
surface area of the leaflets is now exposed to drag which amplifies the force
on the leaflets – drag increases with increasing angle relative to flow. An
analogy is an open door in a drafty corridor: the door starts by moving slowly
and then accelerates as it presents a greater surface area to the wind and
finally it slams shut. The necessary conditions that predispose to SAM are:
anterior position of the mitral valve in the LV, altered LV geometry that
allows flow to strike the mitral valve from behind, and chordal
slack SAM may considered anteriorly directed mitral prolapse In
both conditions the mitral valve is enlarged and is displaced in systole by the
pushing force of flow resulting in mitral regurgitation.
Because the mitral valve leaflet doesn't get pulled into the left
ventricular outflow tract (LVOT) until after the aortic valve opens, the
initial upstroke of the arterial pulse will be normal. When the mitral valve
leaflet gets pushed into the LVOT, the arterial pulse will momentarily collapse
and be followed by a second rise, as the left ventricular pressure overcomes
the increased obstruction that SAM of the mitral valve causes. This can be seen
on the physical examination as a double tap upon palpation of the apical
impulse and as a double pulsation upon palpation of the carotid pulse, known
as bifid pulse.
Screening
HCM is frequently asymptomatic until sudden cardiac death, and is the leading cause of sudden cardiac
death in young athletes. HCM can be detected with an echocardiogram with 80%+ accuracy] which
can be preceded by screening with an electrocardiogram(ECG) to test for heart abnormalities. History and physical
examination alone are ineffective] giving warning of heart
abnormalities in only 3% of patients before sudden cardiac death. One study
found that the incidence of sudden cardiovascular death in young competitive
athletes declined in the Veneto region of Italy by 89% since introduction of
routine Hypertrophic
Cardiomyopathy Screeningof athletes.
United States
There are several potential challenges associated with routine screening
for HCM in the United States. First, the U.S. athlete population of 15 million
is almost twice as large as Italy's estimated athlete population. Second,
these events are extremely rare in the U.S., with fewer than 100 deaths due to
HCM in competitive athletes per year,[ or
about 1 death per 220,000 athletes.
In the United States such screening is not routine and the American Heart
Association has
"consistently opposed" routine screening.Diagnosis
A diagnosis of hypertrophic cardiomyopathy is based upon a number of
features of the disease process. While there is use ofechocardiography, cardiac
catheterization,
or cardiac MRI in the diagnosis of the disease, other
important factors include ECG and genetic test findings and if there is any family
history of HCM or unexplained sudden death in otherwise healthy individuals.
Obstructive and
non-obstructive
Depending on whether the distortion of normal heart anatomy causes
an obstruction of the outflow of blood from the left ventricle of the heart, HCM can be defined as
obstructive or non-obstructive.
§ The obstructive variant of HCM, hypertrophic
obstructive cardiomyopathy (HOCM) has also historically been known as idiopathichypertrophic subaortic stenosis (IHSS) and
asymmetric septal hypertrophy (ASH).
§ Another, non-obstructive variant of HCM is
apical hypertrophic cardiomyopathy, also called Yamaguchi Syndrome or
Yamaguchi Hypertrophy, first described in individuals of Japanese descent.
Physical examination
Differentiating
hypertrophic cardiomyopathy and valvular aortic stenosis
|
||
Aortic
stenosis
|
Hypertrophic
cardiomyopathy
|
|
Echocardiography
|
||
Aortic
valve calcification
|
Common
|
No
|
Dilated
ascending aorta
|
Common
|
Rare
|
Ventricular
hypertrophy
|
Asymmetric, often involving the
septum
|
|
Physical examination
|
||
Common
|
No
|
|
Increased
|
Decreased
|
|
Decreased intensity of murmur
|
Increased intensity of murmur
|
|
Carotid
pulsation
|
Brisk, jerky, or bisferiens pulse
(a collapse of the pulse followed by a secondary rise)
|
|
The physical findings of HCM are associated with the dynamic outflow
obstruction that is often present with this disease.
Upon auscultation, the cardiac murmur will sound similar to the murmur of aortic stenosis. However, a murmur due to HCM will increase in
intensity with any maneuver that decreases the volume of blood in the left
ventricle (such as standing or the strain phase of a Valsalva maneuver). Classically, the murmur is also loudest at the left parasternal
edge, 4th intercostal space, rather than in the aortic area.
If dynamic outflow obstruction exists, physical examination
findings that can be elicited include the pulsus bisferiens and the double apical impulse with each
ventricular contraction. These findings, when present, can help differentiate
HCM from aortic stenosis. In addition, if the individual has premature ventricular
contractions (PVCs), the change
in the carotid pulse intensity in the beat after the PVC can help differentiate
HCM from aortic stenosis. In individuals with HCM, the pulse pressure will
decrease in the beat after the PVC, while in aortic stenosis, the pulse
pressure will increase. However, the murmur intensity increases with both
Aortic Stenosis and HCM post-PVC.
Cardiac catheterization
Pressure tracings demonstrating the
Brockenbrough–Braunwald–Morrow sign
AO = Descending aorta; LV = Left ventricle; ECG = Electrocardiogram.
After the third QRS complex, the ventricle has more time to fill. Since there is more time to fill, the left ventricle will have more volume at the end of diastole (increased preload). Due to the Frank–Starling law of the heart, the contraction of the left ventricle (and pressure generated by the left ventricle) will be greater on the subsequent beat (beat #4 in this picture). Because of the dynamic nature of the outflow obstruction in HCM, the obstruction increases more than the left ventricular pressure increase. This causes a fall in the aortic pressure as the left ventricular pressure rises (seen as the yellow shaded area in the picture).
AO = Descending aorta; LV = Left ventricle; ECG = Electrocardiogram.
After the third QRS complex, the ventricle has more time to fill. Since there is more time to fill, the left ventricle will have more volume at the end of diastole (increased preload). Due to the Frank–Starling law of the heart, the contraction of the left ventricle (and pressure generated by the left ventricle) will be greater on the subsequent beat (beat #4 in this picture). Because of the dynamic nature of the outflow obstruction in HCM, the obstruction increases more than the left ventricular pressure increase. This causes a fall in the aortic pressure as the left ventricular pressure rises (seen as the yellow shaded area in the picture).
Upon cardiac
catheterization, catheters can be placed in the left ventricle and
the ascending aorta, to measure the pressure difference between
these structures. In normal individuals, during ventricular systole, the pressure in the ascending aorta and the
left ventricle will equalize, and the aortic valve is open. In individuals with aortic stenosis or with HCM with an outflow tract
gradient, there will be a pressure gradient (difference) between the left
ventricle and the aorta, with the left ventricular pressure higher than the
aortic pressure. This gradient represents the degree of obstruction that has to
be overcome in order to eject blood from the left ventricle.
The Brockenbrough–Braunwald–Morrow sign is observed in individuals
with HCM with outflow tract gradient. This sign can be used to differentiate
HCM from aortic stenosis. In individuals with aortic stenosis, after a premature ventricular
contraction (PVC), the
following ventricular contraction will be more forceful, and the pressure
generated in the left ventricle will be higher. Because of the fixed
obstruction that the stenotic aortic valve represents, the post-PVC ascending aortic
pressure will increase as well. In individuals with HCM, however, the degree of
obstruction will increase more than the force of contraction will increase in
the post-PVC beat. The result of this is that the left ventricular pressure
increases and the ascending aortic pressure decreases, with an
increase in the LVOT gradient.
While the Brockenbrough–Braunwald–Morrow sign is most dramatically
demonstrated using simultaneous intra-cardiac and intra-aortic catheters, it
can be seen on routine physical examination as a decrease in the pulse pressure
in the post-PVC beat in individuals with HCM.
Treatment
In all patients with hypertrophic cardiomyopathy, risk
stratification is essential to attempt to ascertain which patients are at risk
for sudden cardiac death. In those patients deemed to be at high risk, the
benefits and infrequent complications of implantable cardioverter defibrillator
(ICD) therapy are discussed; devices have been implanted in as many as 15% of
patients at HCM centers.The ICD is the most effective and reliable treatment
option available, harboring the potential for absolute protection and altering
the natural history of this disease in some patients Treatment of symptoms
of obstructive HCM is directed towards decreasing the left ventricular outflow
tract gradient and symptoms of dyspnea, chest pain and syncope. Medical therapy
is successful in the majority of patients. The first medication that is
routinely used is a beta-blocker (metoprolol, atenolol,bisoprolol, propranolol). If symptoms and gradient persist, disopyramide may be added to the beta-blocker. Alternately a calcium channel blocker such
as verapamil may be substituted for a beta blocker. It should be stressed
that most patients' symptoms may be managed medically without needing to resort
to interventions such as surgical septal myectomy, alcohol septal ablation or
pacing. Severe symptoms in non-obstructive HCM may actually be more difficult
to treat because there is no obvious target (obstruction) to treat. Medical
therapy with verapamil and beta-blockade may improve symptoms. Diuretics should be avoided, as they reduce the
intravascular volume of blood, decreasing the amount of blood available to
distend the left ventricular outflow tract, leading to an increase in the
obstruction to the outflow of blood in the left ventricle.
Surgical myectomy
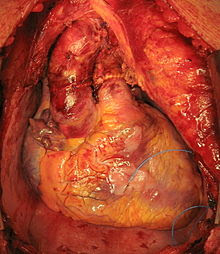
Surgical septal myectomy is an open heart operation done to relieve symptoms in
patients who remain severely symptomatic despite medical therapy. It has
been performed successfully for more than 25 years. Surgical septal myectomy
uniformly decreases left ventricular outflow tract obstruction and improves
symptoms, and in experienced centers has a surgical mortality of less than 1%.
It involves a median sternotomy (general anesthesia, opening the chest, and
cardiopulmonary bypass) and removing a portion of the interventricular
septum. Surgical myectomy resection focused just on the subaortic septum,
to increase the size of the outflow tract to reduce Venturi forces may be
inadequate to abolish systolic anterior motion (SAM) of the anterior leaflet of
the mitral valve. With this limited sort of resection the residual mid-septal
bulge still redirects flow posteriorly: SAM persists because flow still gets
behind the mitral valve. It is only when the deeper portion of the septal bulge
is resected that flow is redirected anteriorly away from the mitral valve,
abolishing SAM. With this in mind, a modification of the Morrow myectomy
termed extended myectomy, mobilization and partial excision of the papillary
muscles has become the excision of choice. In selected patients with
particularly large redundant mitral valves, anterior leaflet plication may be
added to complete separation of the mitral valve and outflow.
Alcohol septal ablation
Alcohol septal
ablation, introduced by Ulrich
Sigwart in 1994, is a percutaneous technique that involves injection of alcohol
into one or more septal branches of the left anterior
descending artery.
This is a technique with results similar to the surgical septal myectomy
procedure but is less invasive, since it does not involve general anaesthesia
and opening of the chest wall and pericardium (which are done in a septal
myomectomy). In a select population with symptoms secondary to a high outflow
tract gradient, alcohol septal ablation can reduce the symptoms of HCM. In
addition, older individuals and those with other medical problems, for whom
surgical myectomy would pose increased procedural risk, would likely benefit
from the lesser invasive septal ablation procedure.
When performed properly, an alcohol septal ablation induces a
controlled heart attack, in which the portion of the interventricular
septum that involves the left ventricular outflow tract is infarcted and will
contract into a scar. Which patients are best served by surgical myectomy,
alcohol septal ablation, or medical therapy is an important topic and one which
is intensely debated in medical scientific circles. Ventricular pacing
The use of a pacemaker has been advocated in a subset of
individuals, in order to cause asynchronous contraction of the left ventricle.
Since the pacemaker activates the interventricular septum before the left
ventricular free wall, the gradient across the left ventricular outflow tract
may decrease. This form of treatment has been shown to provide less relief of
symptoms and less of a reduction in the left ventricular outflow tract gradient
when compared to surgical myectomy.
Cardiac transplantation
Society and culture
Notable cases
In children
While much has been written about adults with HCM, information
regarding children and cardiomyopathy is limited. At this point, it is
estimated 30,000 children are affected by cardiomyopathy of all types (dilated,
hypertrophic, restricted, etc.) Once HCM has been identified in a family,
immediate testing of all family members will help to identify those at risk.
Children often do not show signs of HCM; the first sign many children display
is sudden cardiac arrest. Both invasive and non-invasive techniques exist to
detect thickening of the left ventricle and other abnormalities associated with
HCM. The most common non-invasive diagnostic test for detecting HCM is
electrocardiography, though the most sensitive test for diagnosing HCM is
genetic testing
Beta blockers are often prescribed as the first medical
treatment for HCM in children Many options exist, so if undesirable
side-effects occur a switch can be made.
In other animals
Echocardiography of Hypertrophic-obstructive
cardiomyopathy (HOCM) in a cat.
Feline hypertrophic cardiomyopathy (HCM) is the most common heart disease in cats;
the disease process and genetics are believed to be similar to the disease
in humans.] In Maine Coon and American Shorthair cat breeds, HCM has been confirmed as an
autosomal dominant inherited trait. The first genetic mutation (in cardiac
myosin binding protein C) responsible for feline hypertrophic cardiomyopathy
was discovered in 2005 in Maine Coon cats. A test for this mutation is available. About
one third of Maine Coon cats tested for the mutation have been shown to be
either heterozygous or homozygous for the mutation, although many of these cats
have no clinical signs of the disease. Some Maine Coon cats with clinical
evidence of hypertrophic cardiomyopathy test negative for this mutation,
strongly suggesting that a second mutation exists in the breed. The cardiac
myosin binding protein C mutation identified in Maine Coon cats has not been
found in any other breed of cat with HCM but more recently another myosin
binding protein C mutation has been identified in Ragdoll cats with HCM.
While there is no cure for HCM, early detection and regular
echocardiograms are key to trying to ward off life-threatening problems. Early
signs may include a murmur or even heart failure. Unfortunately, death may
occur without any other signs present, making the disease a difficult and often
deadly one. While medication is commonly given to cats with HCM that have no
clinical signs, no medication has been shown to be helpful at this stage and it
has been shown that an ACE inhibitor is not beneficial until heart failure is
present (at which time a diuretic is most beneficial). Diltiazem generally
produces no demonstrable benefit. Atenolol is commonly administered when systolic
anterior motion of the mitral valve is present.
Thromboembolic disease (TED) is relatively common sequelae of
Feline HCM. The aetiology remains a little uncertain, but it is thought that
ischemic damage to the hypertrophied left ventricular myocardium facilitates
thrombus formation and subsequent embolism. Classically the embolus lodges at
the iliac bifurcation of the aorta, occluding either one or both of the common
iliac arteries. Clinically this presents as a cat with complete loss of
function in one or both hindlimbs. The hindlimbs are cold, and the cat is in
considerable pain. This pain derives from the exaggerated inflammatory response
to the embolus at the point of impact, and the inflammatory mediators released
generally have a vasoconstrictor effect further exacerbating the problem.
Emboli may, rarely, lodge in other locations, typically the renal or
ovarian/testicular arteries as they exit the abdominal aorta.
Treatment of TED is variable - typically very low doses of aspirin
may be prescribed (aspirin however is extremely toxic to cats and should only
be prescribed and administered by a veterinary surgeon). Plavix is also another
widely used drug that may or may not prevent clot formation in HCM cats. The
FATCAT study at Purdue University is addressing the efficacy of aspirin vs.
Plavix for the prevention of a second clot in cats that have already
experienced a clot. Thrombolytic agents (e.g., tissue plasminogen activators)
have been used successfully, but their cost is usually prohibitively high in
veterinary medicine. Despite the relative efficacy of treatment, the prognosis
for cats with TED is poor as they are likely to have significant HCM already,
and a recurrent bout of TED is very likely. For this reason euthanasia is often
considered in TED cats.



No comments:
Post a Comment